We – as a society – had the opportunity to prevent SARS-CoV-2 becoming endemic. We largely wasted it, initially by not locking down early enough or for long enough to remove it from the population. Nor did we use the lockdown period to set up effective data collection, testing, tracking and analytic tools to enable rapid and fine-grained response to predicted changes in incidence (it’s a truism that, by the time you’re working with actual data, you’re already behind in your response).
Public policy decisions are therefore based on incomplete and lagging data, partial models and on individual and committee opinion (however well qualified the participants) rather than being informed by data-driven modelling of potential outcomes. We are also behaving as though we’re dealing with a static target rather than a continuously evolving situation, one where an unintended consequence of partial and incomplete restrictions is that it effectively selects for different strains of the virus, as it evolves to cope with changes in population behaviour. This virus, like any other, has been mutating since before it collided head-on with our species, and it continues to evolve as it seeks selective advantage in exploiting its human host population, at any given time.
The general model of evolution of any virus after it moves from a closed local population to a wider host environment is to become less lethal (if you kill your host off, you reduce your chances of infecting more in a highly connected host population). At the same time though it may become more transmissible. In the case of SARS-CoV-2, that means being selected for more effective cell entry (becoming more infectious) and for lower lethality. And that may be what we’re seeing.
Up to now, the dominant strains of SARS-CoV-2 have relied on the ACE2 enzyme associated with the olfactory neuronal cells to facilitate their entry into the body, so most infections take place via the nose and, to a lesser, extent, other parts of the respiratory tract. There are however now more than 20 significant variants of SARS-CoV-2 in play, and a new swarm of these, under the banner of 20A.EU1, after emerging in Spain in late June, now accounts for more than 80% of cases in the UK and Spain, 60% in Ireland and c.40% in France and Switzerland [Source paper, via ft.com]. At the same time, we’re seeing very high rates of transmission and – relative to the initial period of the pandemic – lower levels of admittance to both general and ICU hospital places.
The mutations in this cluster include some to the ‘spike’ that enables the virus to penetrate host cell walls, and there is some suggestion that these reduce dependency on the ACE2 enzyme, the outcome of which would be that the virus has far more potential entry points to the body. The implications there of course are not only that it is far more infectious but that our new normal of mask wearing and social distancing, based as it is on the transmission of respiratory droplets, may no longer be as effective.
At present it isn’t clear whether the dominance of this variant is because of that increased transmissibility, from visitor movement to and from Spain, or a combination of the two. If however the virus is becoming biochemically more transmissible, we may therefore be seeing a move from the primary vector for infection being respiratory droplets (5-10µm) – typically to mouth, nose, eyes and within a metre or so, and which drop out of the air rather rapidly, to transmission by aerosol (droplets <5µm), which have been found to hang around in the atmosphere for anything between 3 and 16 hours.
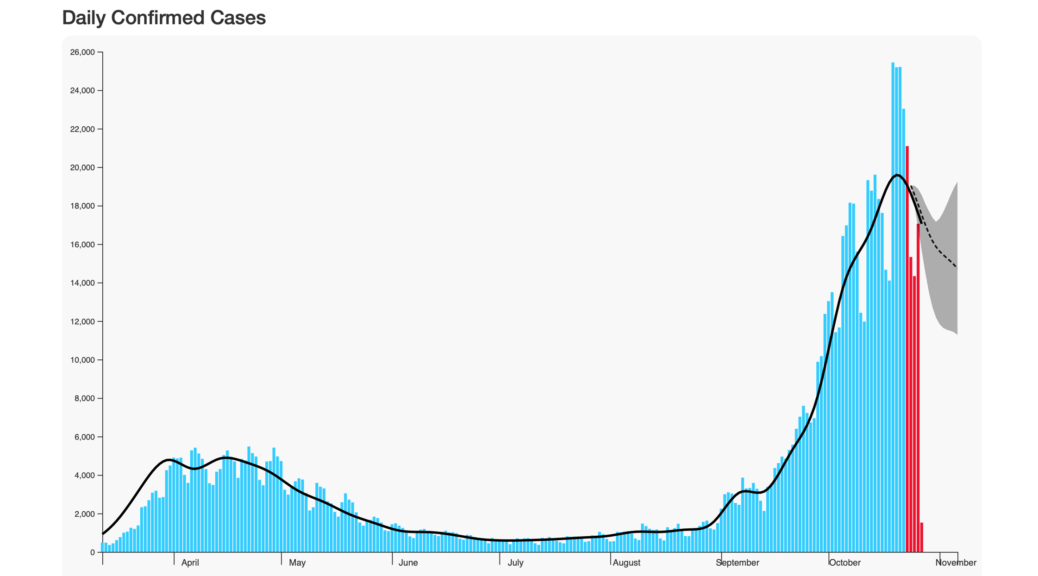
Our own predictive model (see above), which does not yet take into account the epidemiology of new strains, suggests – based on historic data – that a full lockdown now would indeed reduce incidence and, given past and continuing failings, is regrettably necessary. The impact of the new strains however, may well mean that our projections are a tad optimistic so, at the very least, we need to combine specific restrictions with more stringent general social distancing and precautionary measures.
But the dynamic is changing, and what was both necessary and effective in the first peak of Covid-19 may not be either in our current environment. An early, hard and sufficiently long lockdown would have had the lowest social and economic impact over time and might have prevented the virus from becoming endemic. But we didn’t act early enough, hard enough or for long enough, so the time for that model is essentially past – it does appear increasingly likely that SARS-CoV-2 will become endemic, which means that we are going to have to learn to live with it, a situation where repeated lockdowns now are not only likely to prove less effective but, given the shift in the virus itself, they’re the equivalent of repeatedly slamming the stable door to the sound of retreating hooves.
Of the many wasted opportunities in the first six months of the pandemic, failing to develop dynamic mechanisms that would allow us to identify and protect the most vulnerable in society has left us now in the position of now needing that second lockdown. This will inevitably further exacerbate the economic, social and consequential impact of Covid-19. It also risks, thanks to political dogma and ‘ostriching’ (the collective burying of heads in sand to pretend it isn’t happening), locking us further into a long-term, economically and socially disastrous and ineffective roller coaster of lockdown, relaxation and resurgence. So what we can’t be doing is to now lock down without finally putting in place a strategy that will enable us to sustainably mitigate the impact of the pandemic over the long-term: we have to stop pretending that this is something that will be over soon.
If we do develop and put in place rigorous protective and supportive measures for the most vulnerable in society, it will then be possible to follow a lighter and more consistent approach with the wider population: yes, there are risks there – which can be mitigated by more effective testing, tracking and prediction of both the progress and mechanisms of the virus – and we need to be even more rigorous about social distancing and mask wearing, but the overall societal impact would likely to be lower than the imposition of constantly changing and poorly framed restrictions.
The upside (if there is one) of a virus evolving to become endemic is that there is no evolutionary advantage to it of inducing high mortality in its host population. The lower ICU occupancy and lethality we’re seeing will be down to a combination of better understanding of how to treat people effectively, the simple fact that a number of the most vulnerable have already died and – as noted – the virus itself possibly becoming less lethal. We do still need to ensure that we follow a strategy that doesn’t allow both general and ICU bed and staffing capacity to be overwhelmed, so the need for some level of restriction for everyone isn’t going to go away, but the tiered approach, one that inevitably results in full lockdown anyway, does not appear to be appropriate for the future.
All of that is before we start to qualify the test results with the PCR CT value – but that’s for the next post.
Infographic note: the black dotted line in the header graphic is our 14-day UK projection from the data for four days behind the date for which we notionally have data available (we do that due to the volatility of more recent data – the red bars are the data we don’t use in our modelling) and the grey shaded area is our cone of confidence for the projection. You’ll see it’s tracking the more recent data really rather well, almost embarrassingly so, but it does assume that we are following a similar response pattern to the original spike – ie. pretty much a full lockdown, so I’m expecting that, over the next week, our projection will fall below the actual numbers, especially when allowing for the fact that the numbers for the last few days will rise as more data comes in and is published. We also integrate data sets independently from each separate country feed rather than using the UK government’s ‘all UK’ feed, as this has a degree of discrepancy from the individual countries’ data, and has proven rather unreliable in use.
Disclaimer: I am not an epidemiologist, but an erstwhile evolutionary biologist, whose company is now designing (funnily enough) data-driven, emergent analytic and predictive tools for Covid-19. In the course of that, I take input from our epidemiology advisors and try to put their wisdom and our data-driven analysis into a wider context. I may not always succeed.
2020-11-02: This post has been edited to improve clarity of the epidemiological data and outcomes.
Development of Two Worlds’ analytic platform for the Covid-19 pandemic is supported by InnovateUK under R&D grants 54368.